If you’re a Filipino doctor, clinic owner, or telemedicine provider, you know the frustration of paper-based medical records. Finding patient history takes ages, handwriting gets misread, and scheduling is a nightmare. But what if there was a way to streamline everything—patient records, appointments, and operations—without drowning in paperwork? This is where an Electronic Medical Record (EMR) system comes in. A well-structured medical record sample can show you just how much more efficient, secure, and stress-free your practice could be. Let’s break it down and explore why a paperless approach is the future of healthcare.
What is a Medical Record Sample, and Why is it Important?
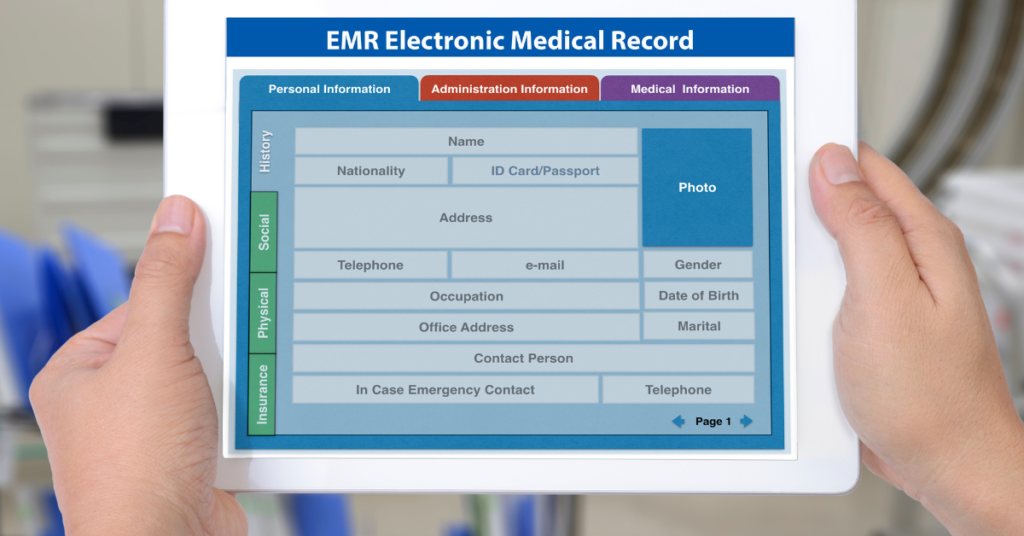
A medical record sample is a structured document containing a patient’s complete health history. It’s not just about keeping things organized—it’s essential for accurate diagnoses, effective treatments, and legal protection.
According to the Expert Institute, incomplete or illegible medical records can lead to misdiagnoses, malpractice claims, and legal issues. A properly structured record ensures that both doctors and patients are protected.
In an EMR system, every entry is clear, searchable, and instantly accessible—no more flipping through stacks of paper!
Key Elements of a Well-Structured Medical Record
A high-quality medical record sample typically includes the following:
1. Patient Demographics
The patient demographics section forms the foundation of any medical record. It contains essential details that help healthcare providers identify and track patient information accurately. This includes the full name, date of birth, gender, and contact details. Additionally, emergency contact information is recorded to ensure immediate communication with a designated relative or guardian in case of medical emergencies.
Beyond identification, demographics play a crucial role in medical history analysis. Factors like age and gender can influence disease risk, medication suitability, and diagnostic approaches. For instance, treatment for hypertension may vary based on age and gender due to differences in physiological response.
Accurate demographic records also streamline patient management in a busy clinic or hospital. When integrated with an EMR system, these details enable seamless appointment scheduling, automatic patient recalls, and efficient billing. Moreover, proper demographic documentation ensures compliance with national health regulations and insurance claims processing.
An EMR system automatically validates and updates patient demographics, reducing the risk of duplicate records and ensuring a smooth patient journey from admission to discharge. In short, this section is the first step toward an organized, efficient, and patient-centric medical practice. Schedule a demo with us if you want to see a medical record sample in action!
2. Chief Complaint & History of Present Illness (HPI)
The chief complaint (CC) is the primary reason a patient seeks medical attention. It is often a short phrase or sentence, such as “persistent chest pain for three days” or “severe headaches with nausea”. This section is crucial for diagnosis because it helps physicians focus on the most urgent medical concerns.
The History of Present Illness (HPI) expands on the chief complaint by providing a detailed narrative of the patient’s symptoms. It typically includes:
- Onset: When did the symptoms begin?
- Duration: How long have they lasted?
- Severity: Mild, moderate, or severe?
- Location: Where is the pain or discomfort felt?
- Aggravating or relieving factors: What makes it better or worse?
- Associated symptoms: Any additional concerns (e.g., fever, dizziness, or weight loss)?
A structured HPI ensures that physicians get a complete picture of the patient’s condition, enabling more accurate diagnoses and treatment plans. EMR systems enhance HPI documentation by allowing quick entry of structured templates, voice dictation, and even AI-powered symptom analysis.
Capturing a thorough, well-documented HPI reduces misdiagnosis risks, improves continuity of care, and ensures high-quality patient management—whether in a hospital, clinic, or telemedicine setting.
3. Medical & Surgical History
A patient’s medical and surgical history provides essential background information for diagnosing current conditions and planning future treatments. This section records past illnesses, chronic conditions, hospitalizations, and previous surgeries. It also includes allergies, which are crucial in preventing adverse drug reactions. Schedule a demo with us to see what this looks like in a medical record sample.
A well-documented medical history typically includes:
- Chronic diseases: Hypertension, diabetes, asthma, etc.
- Past infections: Tuberculosis, hepatitis, dengue fever, etc.
- Family history: Hereditary conditions like heart disease or cancer.
- Mental health history: Depression, anxiety, or psychiatric disorders.
The surgical history covers any past procedures, from minor outpatient surgeries to major operations like heart bypasses or organ transplants. Physicians use this information to assess surgical risks, medication interactions, and recovery expectations.
With an EMR system, medical and surgical histories are easily accessible and constantly updated, preventing redundant tests and improving decision-making efficiency. This helps doctors predict complications, personalize treatment plans, and avoid harmful medication interactions. A structured, digital record ensures continuity of care, especially when a patient consults multiple specialists.
4. Medications & Allergies
The medications & allergies section ensures safe prescribing practices and helps prevent adverse drug interactions. This part of the medical record contains:
- Current prescriptions: Name, dosage, frequency, and duration.
- Over-the-counter medications: Vitamins, supplements, and herbal remedies.
- Past medications: Treatments previously tried, discontinued, or failed.
- Allergies: Drug, food, and environmental allergies with reaction severity.
Medication errors are a leading cause of preventable patient harm, especially in busy clinics or hospitals. Illegible handwriting, dosage misinterpretations, and medication duplications can lead to serious complications. An EMR system automatically checks for drug interactions, contraindications, and allergy warnings, significantly reducing medical errors.
For telemedicine and chronic disease management, automated medication reminders and prescription renewalsensure patients stay compliant with their treatments. Additionally, integrated e-prescription features enable direct digital communication with pharmacies, reducing wait times and improving patient convenience.
Ultimately, a well-documented medications & allergies section safeguards patients from unnecessary risks and ensures precise, evidence-based treatment decisions.
5. Physical Examination & Vital Signs
The physical examination & vital signs section records objective findings from a patient’s visit. This includes:
- Vital signs: Blood pressure, heart rate, temperature, respiratory rate, and oxygen saturation.
- General appearance: Signs of distress, consciousness level, or abnormalities.
- System-specific findings: Cardiovascular, respiratory, neurological, or gastrointestinal observations.
Tracking vital signs over time helps detect trends and early warning signs of disease. A sudden spike in blood pressure, for example, may indicate worsening hypertension, while consistently low oxygen levels could suggest respiratory distress.
Using an EMR system, physicians can chart trends, set alerts for abnormal values, and integrate data from digital devices like blood pressure monitors and pulse oximeters. This not only enhances monitoring accuracy but also facilitates remote patient management.
Well-documented physical exams allow better clinical decision-making, early disease detection, and improved patient safety, ensuring timely interventions when needed. Would you like to see a medical record sample for your practice? Schedule a demo with us!
6. Diagnosis & Treatment Plan
The diagnosis & treatment plan section outlines the doctor’s medical assessment and prescribed course of action. A proper diagnosis considers patient history, examination findings, lab results, and imaging studies.
This section typically includes:
- Primary diagnosis: The confirmed condition based on evidence.
- Differential diagnosis: Other possible conditions being ruled out.
- Recommended treatment: Medications, lifestyle changes, therapy, or referrals.
- Follow-up instructions: When the patient should return or undergo further testing.
An EMR system simplifies diagnosis documentation by providing preloaded templates, AI-driven diagnostic suggestions, and clinical decision support tools. This ensures standardized, evidence-based treatment planning for better patient outcomes.
With automated follow-up reminders, patients stay on track, reducing missed appointments and improving chronic disease management.
7. Laboratory & Imaging Results
Lab tests and imaging studies play a crucial role in diagnosing and monitoring conditions. This section includes:
- Blood tests: CBC, lipid profile, blood sugar levels, etc.
- Imaging: X-rays, CT scans, MRIs, and ultrasounds.
- Microbiology & pathology reports: Biopsy results, cultures, etc.
A paper-based system often results in lost reports or delayed diagnosis. With an EMR system, lab results are instantly updated, reducing waiting times and ensuring prompt treatment decisions.
Real-time data access also helps prevent redundant tests, reducing costs and improving efficiency. Additionally, patients can view their results via secure patient portals, enhancing transparency and engagement in their health.
8. Physician Notes & Follow-Ups
A patient’s journey doesn’t end after one visit. Physician notes and follow-ups ensure continuity of care. This section includes:
- Progress notes: Updates on symptoms, treatments, and responses.
- Follow-up plans: Next visit dates and additional tests.
- Referrals: Specialist recommendations.
An EMR system keeps a chronological record of patient visits, allowing physicians to track treatment progress, detect recurring issues, and adjust care plans accordingly.
Additionally, automated appointment reminders and telehealth integration improve patient compliance, ensuring faster recoveries and better long-term health outcomes.
A well-documented medical record isn’t just for organization—it directly improves patient safety and treatment efficiency.
The Shift to EMR: Why Filipino Healthcare Needs It
📌 1. Saves Time and Eliminates Paperwork
A 2022 study published in the Journal of Medical Systems found that EMRs reduce documentation time by 45%, allowing doctors to focus on patient care instead of paperwork. With an EMR, searching for past records takes seconds, not hours.
📌 2. Enhances Patient Safety
Illegible handwriting leads to medication errors, a major concern in Filipino healthcare settings. Digital prescriptionsremove this risk entirely. Plus, built-in alerts notify doctors of potential drug interactions or allergies.
📌 3. Improves Scheduling and Reduces No-Shows
With an EMR-integrated scheduling system, clinics can send automated appointment reminders. This alone can reduce missed appointments by 38%, according to a study by the National Center for Biotechnology Information (NCBI).
📌 4. Supports Telemedicine & Remote Access
For Filipino healthcare providers offering telemedicine, an EMR ensures secure, real-time access to patient history, lab results, and prescriptions—anytime, anywhere.
📌 5. Strengthens Legal Protection
According to the Expert Institute, poorly documented records are a top reason for malpractice claims. An EMR provides timestamped, organized records that safeguard against legal risks.
How an EMR System Transforms Medical Records in Practice
A medical record sample in an EMR system is more than just digitized paperwork. It’s a game-changer in clinic efficiency. Imagine this:
- A patient walks in, and their entire medical history is accessible in one click.
- You prescribe medication, and the system automatically checks for allergies.
- Lab results are updated in real-time—no more lost paperwork.
- Follow-ups are scheduled automatically with SMS reminders.
This is the kind of seamless experience an EMR system offers.
Choosing the Right EMR System for Your Practice
Not all EMRs are the same. Here’s what to look for:
- User-Friendly Interface – If it’s complicated, doctors and staff won’t use it.
- Customizable Templates – Pre-set forms for different specialties save time.
- Secure & Compliant – Ensures patient confidentiality under Philippine Data Privacy Laws.
- Integration with Billing & Telemedicine – A complete practice management solution.
- Cloud-Based Accessibility – Access patient data anywhere, anytime.
See an Medical Record Sample in Action – Try a Free Demo
Still relying on paper records? It’s time for a change.
- Book a FREE demo today: Schedule a Demo
- Watch how an EMR works: Video Tutorials
- Learn more: Doktor EMR
The future of healthcare is digital. Are you ready to make the switch?